Dr. Harshit is an emergency medicine physician, working on the floor through this pandemic. He offers an algorithm to help deal with the onslaught we face as healthcare workers on the ground.
Please note that this will help if multiple institutions across cities follow a standardised guideline and cooperate with each other to manage the pandemic.
Based on the proposed guidelines for Coronavirus response by the Government of Karnataka, we came up with this simple algorithm for better understanding – For the public and healthcare professionals (HCP). Because the first problem lies there itself. Just not good enough understanding of what is to be done by individuals in the system.
This algorithm is quiet simple and works. If :-
- Properly followed and involved personnel are trained
- Issues foreseen and taken care of
- Enforcement and monitoring continuously that it is being followed without corruption
- Transparency to the public and accountability by the system
- Allowing room for expansion as the situation worsens. Because it will definitely worsen before it improves. As we are witnessing in other badly hit metropolitan cities.
As HCP’s on the frontlines seeing the daily ground reality problems we wanted to outline certain major problem points in this algorithm that need to be taken care of at the earliest.
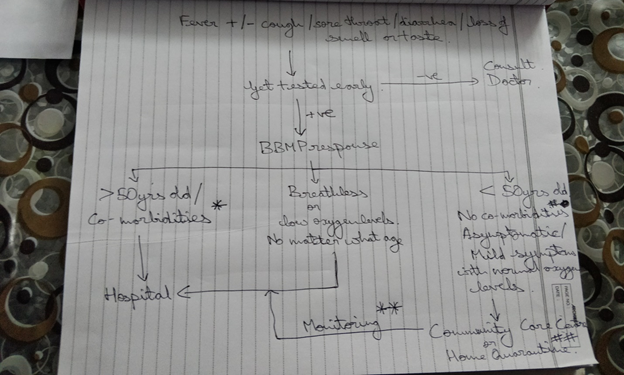
*pre-existing co-morbidities like Lung diseases/ TB/ Liver disease/ Heart disease/ Kidney disease/ Patient on dialysis/ HIV/ Cancer/ Patient on steroids or other immunosupressants/ Immuno-compromised patients
#co-morbidities like Hypertension/ Diabetes/ Thyroid disorders/ Obesity do not necessarily need to be admitted. Left to the discretion of consulting physician
## The decision of home quarantine or placing a patient in a Community Care Centre (CCC) will be made on assessment based on treating physicians discretion, Living situation of the patient – can the patient isolate, availability of a family member to monitor, etc.
** Monitor for symptoms like breathlessness, blue-ish discolouration of lips or fingers or toes, chest tightness, altered sensorium, low oxygen saturation <95% on oximeter, etc.
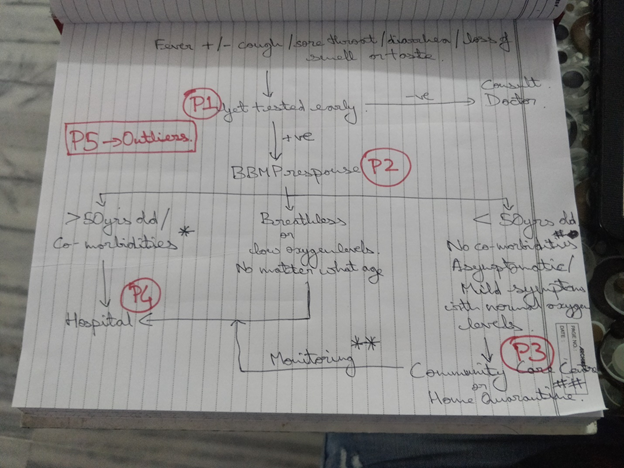
P1 – Symptomatic person or primary contacts of a COVID positive person not getting tested at the earliest on symptom onset. Most people, out of fear of isolation and quarantine, do not seem to be getting themselves tested. Our advice to people is if you have symptoms please get tested early – this way if you test positive you are in the system. It is the systems responsibility then to monitor you at home or get you a hospital bed if you are in need of it, which currently is the major problem. Do not wait till you get really sick because then getting a bed currently is next to impossible as the system will not take responsibility for you. And the getting tested, getting a report and getting a hospital bed after that might be too late.
Availability of testing does not seem to be a problem anymore. Capping of prices of the testing from different labs needs to be looked at as this would help the poor get tested.
P2 – You may get tested but due to the load of testing most labs take 48 hours to 120 hours to report your sample. And now the new rule from the government directing labs to not give the reports to the patients, only release it to BBMP. And then BBMP will respond and go to the patient and assess the situation and either decide on home quarantine / CCC/ Hospital. Which again, lets say the report was ready in 48 hours and dispatched to BBMP, but simply due to the load BBMP has to handle they take another 48 hours to 144 hours to respond (this 144hours happened with one of my own family members).
Let me illustrate this problem to you with a real scenario that happened a few days ago in the hospital we work at. A lady from Chintamani Mrs. M developed fever and cough on 26th of June. Got tested on 27th of June. Developed breathlessness on 29th of June. Went to a hospital but they would not admit her without a report so she went to the testing centre where she got swabbed and they wouldn’t release her the reports and told her to contact BBMP. Which they tried and there was no response from BBMP. She went from hospital to hospital for 2 days and everywhere the same answer – “get us the report and an official letter from BBMP if its positive only then we can give you a bed”. She came to us in Bengaluru on the 1st of July already dead in the ambulance. See the problem there???
P3 – This on paper is a very sorted out plan with guidelines and everything on when are you home quarantined and when are you taken to a CCC. Reality of it we really don’t know if it is good or bad. But like I said foreseeing the problems that may present is a big part of our success in responding to this pandemic.
The CCC’s must have HCP’s monitoring patients regularly so if they worsen can be taken to a hospital at the earliest. These HCP’s must be trained in what to assess for and it must be documented. Patients on home quarantine must be assessed and trained properly in monitoring themselves. So should their family members who will play the role of primary caregivers. Proper counseling and monitoring that the patient must not pass on the infection to others in the family or the community must be taken care of. If the patient develops symptoms on monitoring as per guidelines that need the patient to be taken to a hospital, a hospital of response must already be assigned for every home quarantined patient. Monitoring of these patients on home quarantine by HCP’s must be done daily. The startups vs COVID initiative and the apthamitra app can be used for the same.
P4 – Now this is the biggest problem.
- Hospitals not holding beds for coronavirus patients as much as directed by government guidelines.
- Government not enforcing these hospitals to release beds for these patients and not monitoring the same.
- Patients who should be home quarantined or in CCC’s taking up hospital beds by using forces of connections and money.
- Capping of prices as per government guidelines to be followed strictly and monitored. Beds are being sold off to patients who can afford it and don’t need a hospital bed. Whereas patients who can’t afford it and need the bed are not able to get any.
- Patients not on ventilators and only on oxygen are taking up ICU beds in private hospitals as they would profit more from it. This makes already scarce ICU beds and ventilators even more scarce because of wrong use of ICU beds. For some reason government price capping guidelines has allowed a column for ICU beds without ventilator. That should not be allowed in a pandemic of this scale – ICU beds means with ventilator only. If not on ventilator and only on oxygen requiring strict monitoring patient must be kept in High Dependence Units (HDU’s).
- Maintaining transparency of bed availability to the public in real time. And these hospitals held accountable for not caring for sick patients and sending them away from the door.
- As the situation gets worse, which it will before it gets better, there must be a plan already in place to expand the current existing number of hospital beds, ICU beds and ventialtors. When the current assigned numbers are already TRULY AND ACTUALLY full.
All of this gets solved only by two methods. A Centralised Bed Allocation System (CBAS) and a grievances helpline number. There are way too many sick patients running from door to door of hospitals without any help and accountability and dying on the streets. The government has said they are working on a CBAS but how it should ideally work is a different ball game. We will outline that in our next write-up, based on ground reality as no one seems to be asking us what the real problem is but only making PR announcements that all izz well. Well no, all izz not really well.
P5 – These are your SARI patients. Severe Acute Respiratory Illness – not tested for COVID but breathless, and given a pandemic situation all breathless patients must be treated as suspect COVID’s. The government uptill now seems to think they don’t have a responsibility to these patients as they did not get tested. The guidelines earlier released by the GoK to hospitals to reserve beds mentioned only COVID positive patients. Hospitals have been using that technicality to avoid taking patients of SARI and asking them for a report first and a BBMP letter saying this patient is assigned to this hospital. Even government institutes like Bowring and Victoria are exclusively for COVID positive tested and reported patients only.
Let me illustrate this with another short story. We got a patient yesterday Mr. J who has been breathless since 2 days and been from hospital to hospital (12 of them) for a bed for his breathlessness. Shunted everywhere saying first go get tested and bring us the report only then we can give you a bed. He was pronounced dead in the ambulance itself by us. We tested him after and put the body in the mortuary. It was positive but well what is the point now right.
The reserved beds must have separate isolation areas for suspected SARI patients and cared for appropriately while awaiting reports. And once report is available shift the patient to the appropriate area of care. These patients should also be able to connect to the CBAS and the grievances helpline number to be able to get care.
There are government guidelines been announced and most are very sound. But till we take individual responsibility as patients, government officials, administrators of hospitals and HCP’s – none of it works. Let us all ask the right questions to the right people to make a difference. Transparency and accountability is key. And the ability to expand and adapt as the situation changes.
Dr. Harshit Mundra
